What is the Role of a Neurologist among Mental Health?: Expert Insight.
A neurologist plays a crucial role in diagnosing and treating brain-related mental health disorders. They specialize in conditions that affect the nervous system and influence mental health.
Neurologists, medical doctors specialized in disorders of the nervous system, represent a critical component of the multidisciplinary approach to mental health care. Their expertise extends to a range of conditions, from migraines and epilepsy to more complex neurological disorders such as Parkinson’s disease and multiple sclerosis, which can have profound psychological implications.
By employing a variety of diagnostic tools, including EEGs, MRIs, and clinical evaluations, neurologists can identify neurological conditions that may manifest as or contribute to mental health issues. As part of a collaborative care team, they work closely with psychiatrists, psychologists, and other health care professionals to develop comprehensive treatment plans, offering a blend of medication management, lifestyle recommendations, and in some cases, referral for psychological services or complimentary therapies. Emphasizing early diagnosis and intervention, neurologists are vital in ensuring patients receive tailored, effective treatment that addresses both the neurological and psychological aspects of their well-being.

Credit: www.post-gazette.com
The Nexus Of Neurology And Mental Health
Neurologists play a key role in understanding mental health. These experts study the brain and its connection to behavior and cognition. Many believe that only psychiatrists treat mental disorders. This is not true.
Neurologists and psychiatrists often work together. They look at how brain disorders affect the mind. Neurological conditions like Epilepsy or Parkinson’s can cause mental symptoms. Hence, understanding brain functions helps in mental health care.
People must know that brain health influences emotions and behaviors. Without this knowledge, treatment could miss important causes. The brain science behind mental illness is complex. Yet, it is vital for effective treatment plans.
Who Is A Neurologist?
A neurologist specializes in the brain and nervous system. They deal with various brain disorders that can affect mental health. These experts spend many years in school. First, they must complete college and medical school. Next, they do an internship. After that, they spend several years in a neurology residency program. This training gives them deep knowledge of the brain.
Neurologists often focus on one area of the brain. This is a subspecialty. For example, some may specialize in child neurology. Others might focus on sleep disorders. They may also deal with epilepsy, movement disorders, or migraines. Neurologists use their skills to diagnose and treat many brain health issues. This is crucial for our mental well-being.
Differentiating Psychiatrists And Neurologists
Neurologists and psychiatrists both deal with mental health. The roles they play may overlap. Neurologists focus on brain disorders. They treat things like epilepsy, strokes, and migraines.
Psychiatrists handle mental illnesses. They care for patients with depression, anxiety, and schizophrenia. These two kinds of doctors will often work together. They help patients with complex conditions that affect the brain and mind.
Neurologists may use brain scans to learn about diseases. Psychiatrists may talk more to understand feelings. They use tests to know how the mind works. With this knowledge, they can plan the best treatment. They make sure each patient gets the proper help.

Credit: drraoshospitals.com
Common Neurological Disorders With Psychological Symptomatology
Neurologists play a pivotal role in diagnosing and treating disorders where mental health intertwines with the nervous system. Conditions such as Epilepsy can significantly impact mood, often manifesting in heightened anxiety or depression. It’s not just physical symptoms that need attention but also these psychological changes.
Dementia is another key area within a neurologist’s expertise, where cognitive decline is the hallmark. Memory loss and impaired judgment are common threads, necessitating comprehensive care that addresses both the mental and neurological facets.
Neurologist’s Role In Diagnosis
Neurologists play a pivotal role in understanding how the brain impacts mental health. They use neuroimaging techniques like MRI and CT scans. These scans reveal vital information about brain structure and function. Such images can show changes linked to mental health issues.
These experts also perform neurological assessments tailored for psychiatric conditions. Tests can include evaluating memory, reasoning, and emotional processing. These assessments help identify neurological contributions to mental disorders. This leads to more accurate diagnoses for patients.
Treatment Modalities Used By Neurologists
Neurologists specialize in treating brain and nervous system diseases. Medications play a key role in managing conditions like epilepsy, migraines, and multiple sclerosis. They choose the best drugs for each patient’s needs.
Emerging therapies offer new hope in brain health. Techniques such as deep brain stimulation (DBS) are gaining attention. DBS can help control movement disorders. It may benefit those with Parkinson’s disease.
| Therapy Type | Conditions Treated | Notes |
|---|---|---|
| Medication | Epilepsy, Migraines, Multiple Sclerosis | Customized to patient |
| Deep Brain Stimulation | Parkinson’s Disease | Controls movement |
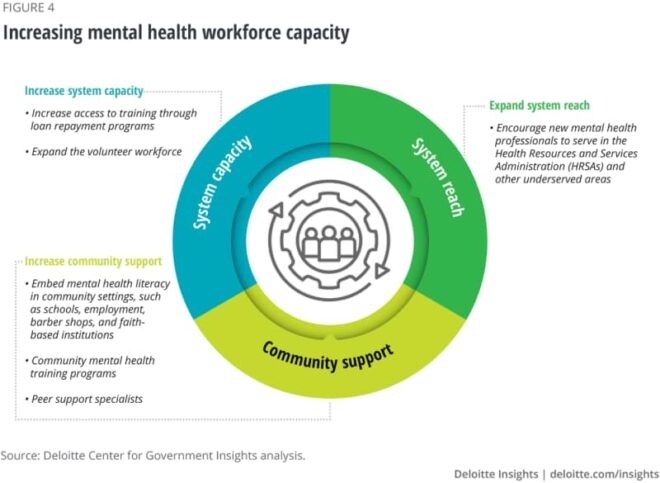
Interdisciplinary Approaches To Mental Health
Neurologists play crucial roles within mental health teams. They often work closely with psychiatrists, psychologists, and other healthcare professionals. Together, they tackle complex brain-related conditions. Mental health challenges frequently demand this teamwork approach.
Effective treatment often relies on Collaborative Care Models. This method includes various experts who focus on different health areas. Such teamwork leads to better patient outcomes. Neurologists bring a deep understanding of brain function to the table.
| Year | Integration Example | Result |
|---|---|---|
| 2018 | Memory Clinic with neurologists | Improved patient satisfaction |
| 2020 | Depression center with neurology unit | Quicker diagnosis and treatment |
A look at case studies shows success with integration. One study highlighted a clinic where neurologists and mental health experts worked together. Patients got better care. Another case showed faster help for depression with neurologists involved.
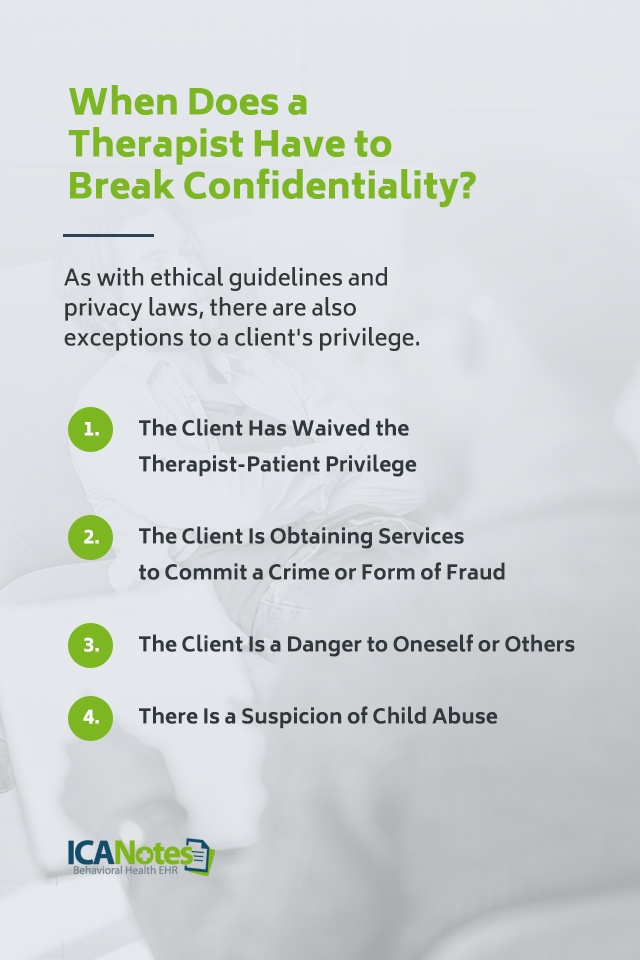
Challenges And Ethical Considerations In Neurology And Psychiatry
Neurologists play a crucial part in understanding the brain regarding mental health. They face many challenges and ethical questions. One key issue is the stigma and misunderstanding around mental illnesses. This leads to patients often feeling ashamed. They may avoid seeking the help they need. Education and awareness are important to change this.
Looking ahead, the field of neurological psychiatry is evolving. New technology and research give hope for better treatments. It’s a field that promises to improve the lives of many in the future. Experts are working hard to combine knowledge from both neurology and psychiatry. This blend aims to tackle brain health in a more holistic way.
“`
Advancing Research And Treatment In Neurology For Mental Health
Neurologists are key players in improving mental health through research. They work hard to understand the brain. By studying the brain, they find new ways to help patients. Proper mental health care needs their expertise.
New research in neuroscience shows exciting progress. Scientists think they might cure some brain diseases soon. They are testing new drugs and therapies now. Breakthroughs could happen any day.
| Research Area | Details |
|---|---|
| Brain Mapping | Doctors see inside the brain better. |
| Genetic Studies | They find links between genes and mental health. |
| New Medications | Patients could get better with new pills. |

Credit: www.parkview.com
Frequently Asked Questions For What Is The Role Of A Neurologist Among Mental Health?
What Is The Role Of Neurologist Among Mental Health Professionals?
A neurologist specializes in disorders of the nervous system, often consulting on mental health issues linked to neurological conditions. Their role is diagnostic and consultative, focusing on brain health impacts on behavior and cognitive functions.
What Does A Neurologist Do For Mental Health?
A neurologist diagnoses and treats disorders affecting the brain, spinal cord, and nerves, which can impact mental health. They manage neurological conditions that may have psychiatric symptoms, supporting overall mental wellness.
What Is The Role Of Neuroscience In Mental Health?
Neuroscience plays a crucial role in mental health by uncovering how brain function impacts behavior and emotions. This insight aids in developing effective treatments and interventions for various mental health conditions.
What Is The Role Of A Neurologist Among Mental Health Professionals Brainly?
A neurologist specializes in diagnosing and treating neurological disorders affecting the brain and nervous system, complementing mental health care.
Conclusion
Navigating the complexities of mental health often leads to a neurologist’s door. These specialists play a pivotal role in diagnosing and treating neurological disorders that impact mental well-being. They bridge gaps in understanding how brain functionality relates to mental health issues.
Seeking a neurologist’s expertise can be a critical step in obtaining comprehensive care and fostering holistic healing for those battling with neurological contributions to mental ailments.