How to Become a Mental Health Counselor: Unlock Your Inner Healing Potential
To become a mental health counselor, earn a master’s degree in counseling and obtain state licensure. Embarking on a fulfilling career as a mental health counselor requires dedication and commitment.
By obtaining a master’s degree in counseling and meeting state licensing requirements, individuals can make a positive impact on the lives of those struggling with mental health issues. In addition to formal education, gaining practical experience through internships and licensure exams are crucial steps towards becoming a successful mental health counselor.
As the demand for mental health services continues to rise, pursuing a career in this field offers opportunities for personal growth and professional development. By providing empathetic and effective counseling, mental health counselors play a vital role in supporting individuals on their journey to improved mental wellness.

Credit: www.amazon.com
The Path To Mental Health Counseling
Embarking on the path to mental health counseling entails obtaining a bachelor’s degree in psychology or a related field, followed by a master’s program in counseling. Prospective counselors must also complete supervised clinical experience and fulfill state-specific licensing requirements. Continuous professional development through workshops and seminars is also essential for maintaining counseling credentials.
| The path to becoming a Mental Health Counselor involves Education and Training. |
| Completing a master’s degree program in counseling or related field is essential. |
| After acquiring the necessary education, obtaining Licensing and Certification is crucial. |
| Each state has specific requirements that must be met to practice as a counselor. |
Developing Essential Skills
Empathy and Active Listening: One of the key skills a mental health counselor should possess is empathy. Being able to understand and share the feelings of clients creates a safe and supportive environment for them to open up. Active listening is also crucial in order to fully comprehend their experiences and concerns. It involves giving full attention to the client, and using verbal and non-verbal cues to show that you are present and engaged.
Cultural Competence: Another essential skill is cultural competence, which involves understanding and respecting the diversity of clients’ cultural backgrounds. This includes having awareness of different cultural values, beliefs, and practices, and being able to adjust the counseling approach accordingly. By being culturally competent, mental health counselors can ensure that they are providing appropriate and effective care to clients from a variety of backgrounds.
Gaining Experience And Expertise
To become a mental health counselor, gaining experience and expertise is crucial. One way to gain practical experience is through an internship and supervised practice. These opportunities allow aspiring counselors to work under the guidance and supervision of experienced professionals. Additionally, specialized training can provide further expertise in specific areas of mental health counseling. This can include courses and workshops that focus on various therapeutic approaches, such as cognitive-behavioral therapy or trauma-informed care. By actively seeking out these opportunities and continually expanding knowledge and skills, individuals can become well-equipped to help clients navigate their mental health challenges.

Credit: esoftskills.com
Navigating The Job Market
When pursuing a career as a mental health counselor, it’s essential to consider the various job opportunities available. You can choose to work in a private practice or within an institution. In a private practice, you have the flexibility to set your own schedule and specialize in specific areas of interest. On the other hand, working in an institution may provide more job security and benefits. It’s important to weigh the pros and cons of each option to determine which path aligns best with your career goals.
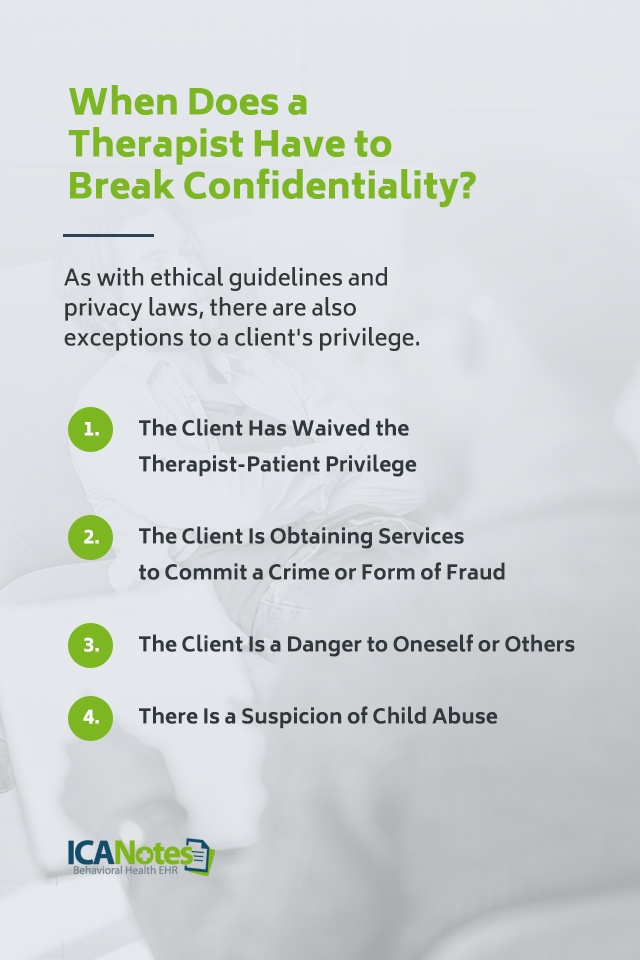
Understanding Ethical And Legal Standards
Mental health counselors must adhere to ethical and legal standards for practice. Confidentiality is crucial to protect clients’ privacy. Informed consent ensures clients understand the counseling process.
Self-care And Burnout Prevention
Taking care of yourself is crucial in the field of mental health counseling. As a counselor, you often spend your time caring for others, which can lead to burnout if you neglect your own needs. Self-care is important because it helps you maintain your emotional well-being and prevent burnout.
Recognizing the symptoms of burnout is also essential. Some common signs include exhaustion, cynicism, and reduced effectiveness in your work. Taking time to rest and recharge is vital to prevent burnout. It’s important to set boundaries and prioritize self-care activities such as exercise, relaxation techniques, and seeking support from friends and family.
Embracing Holistic Approach
Becoming a Mental Health Counselor involves embracing a holistic approach. This means focusing on mindfulness and meditation techniques to support clients’ well-being. Integrating alternative therapies such as art or music can enhance the counseling experience.
Advocacy And Progression In Mental Health
In the field of mental health counseling, advocacy and progression play a crucial role in promoting mental health awareness. Counselors have the opportunity to advocate for their clients and the wider community, striving to destigmatize mental health issues and ensure access to quality care. This includes raising awareness of different mental health conditions and the importance of early intervention and treatment. Furthermore, counselors can contribute to policy and research, actively participating in the development of mental health policies and programs. By staying up-to-date with the latest research and best practices, counselors can enhance their knowledge and skills to better serve their clients. Through their dedication and efforts, mental health counselors pave the way for a more inclusive and compassionate society, where individuals can seek help without fear or judgment.

Credit: www.facebook.com
Frequently Asked Questions On How To Become A Mental Health Counselor
How Long Does It Take To Become A Mental Health Counselor In Texas?
It takes about 6-8 years to become a mental health counselor in Texas. This involves obtaining a bachelor’s degree, completing a master’s program in counseling, gaining supervised experience, and passing the state licensure exam.
What Is The Difference Between A Counselor And A Therapist?
Counselors primarily focus on short-term goals and practical solutions, while therapists delve into deeper emotional issues for long-term growth.
What Do You Need To Be A Mental Health Therapist In Texas?
To be a mental health therapist in Texas, you need a master’s degree in counseling or a related field. You must also accumulate supervised experience and pass the licensing exam conducted by the Texas State Board of Examiners of Professional Counselors.
How Do I Become A Counselor In Nebraska?
To become a counselor in Nebraska, follow these steps: 1. Earn a bachelor’s degree in psychology or a related field. 2. Complete a master’s degree in counseling or a similar program. 3. Gain supervised clinical experience through internships or practicums. 4.
Obtain state licensure by meeting Nebraska’s specific requirements. 5. Consider pursuing additional certifications or specializations for career advancement.
Conclusion
In your journey to become a mental health counselor, dedication, compassion, and continuous learning are key. Embrace challenges and always prioritize self-care. Stay updated with the latest research and training opportunities. Remember, your impact on others’ well-being is profound. Stay committed to this rewarding profession.