Under What Circumstances Can Mental Health Pros Breach Privacy?
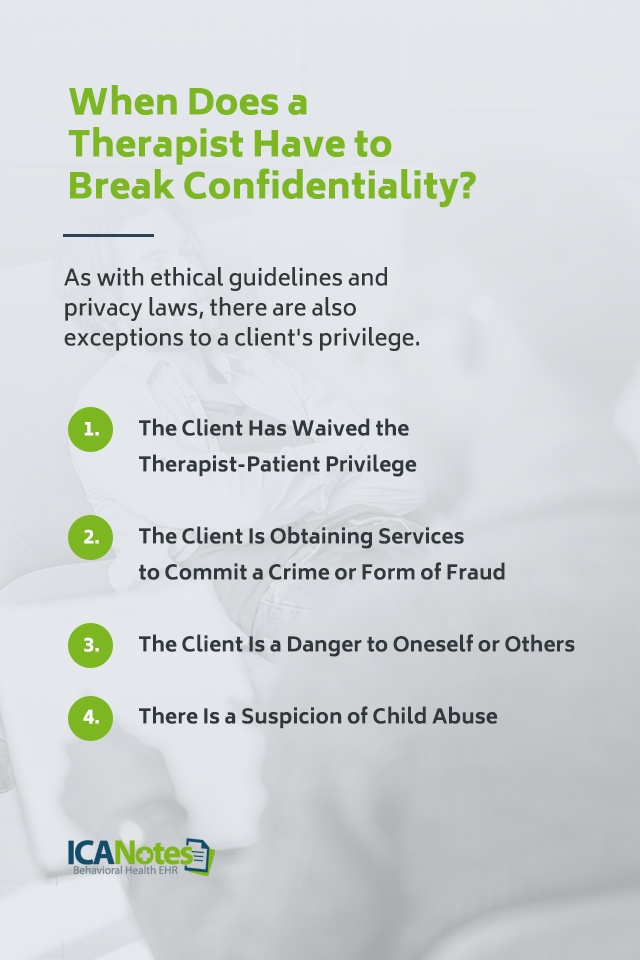
Mental health professionals may break confidentiality if there’s an imminent threat to someone’s safety or as required by law. This includes situations of potential harm to the client or others, child abuse, and court orders.
Confidentiality is a cornerstone of mental health care, establishing trust between clients and therapists. Yet, situations arise where professionals must balance ethical obligations with legal requirements, potentially overriding their commitment to privacy. In such instances, therapists navigate complex professional guidelines to protect their clients’ well-being and comply with legal mandates.
The criteria for breaching confidentiality are strict, ensuring that privacy is maintained unless substantial evidence exists that not doing so could result in harm. Mental health practitioners receive training to identify these scenarios, ensuring they act with care and due diligence. Understanding the limits of confidentiality is essential for anyone engaging in therapy, reinforcing the promise of a safe space with clear boundaries.
Confidentiality In Mental Health Care
Mental health professionals pledge to protect client privacy. The ethical duty of non-disclosure binds them. This means they must keep secrets safe.
Yet, certain laws may force therapists to break silence. Examples include plans for harm to oneself or others, child abuse, and court orders. Their duty is to protect clients and the public.
| Condition | Action Required |
|---|---|
| Threat to Self | Report to authorities for safety. |
| Threat to Others | Warn potential victim or police. |
| Child Abuse | Notify child protection services. |
| Court Orders | Release information as required. |
Informed Consent And Limits Of Privacy
Mental health professionals value patient privacy highly. Informed consent is when patients agree to share details. They learn about privacy limits before treatment starts. Not all situations need consent for confidentiality breaks. Legal requirements may force therapists to share information. This includes cases with imminent harm or abuse reports. Court orders can also demand a breach of privacy. Professional duty may override client secrets to protect someone.
Medical emergencies sometimes mean info is shared. This is without a client saying yes. Public safety concerns also allow for rare privacy breaks. Ethical guidelines help professionals decide. They ensure decisions are careful and just.
Imminent Danger To Self Or Others
Mental health professionals must assess the threat level when a client poses imminent danger. A serious threat to self or others may lead to a confidentiality breach. Specific steps are taken to determine the danger’s immediacy.
An evaluation of the threat includes the intention, means, and plan to hurt oneself or others. This assessment helps professionals decide on the need for immediate action.
Abuse Or Neglect Reporting
Mental health professionals must follow strict confidentiality rules. Yet, certain situations legally compel them to disclose confidential information. Protecting vulnerable populations is paramount. Among these situations are cases where abuse or neglect of children or the elderly is suspected.
| Scenario | Action Required |
|---|---|
| Child abuse | Professionals must report to authorities |
| Elder neglect | Reporting is also a legal duty |
| Domestic violence | May need to report if vulnerable persons are involved |
These legal obligations ensure the safety of those who cannot protect themselves. Professionals balance confidentiality with legal responsibilities. They aim to prevent harm while still providing care. Thus, in certain circumstances, breaking confidentiality is not only allowed but required.
Legal Proceedings And Court Orders
Mental health professionals hold a duty to maintain client confidentiality. Legal scenarios, however, sometimes require them to disclose information. Court orders and subpoenas can compel therapists to share client records. It’s crucial to note that strict legal standards must be met for these disclosures.
| Confidentiality Break | Reason |
| Court Order | Judge’s direct request |
| Subpoena | Legal document requiring evidence |
It’s essential for mental health experts to navigate legal complexities cautiously. They must weigh their duty to their clients against legal obligations. Disclosure is rare and often contested to protect client privacy.

Credit: www.hipaajournal.com
Duty To Warn And Protect
The Tarasoff ruling sets a precedent for mental health professionals. It requires them to notify potential victims if a client poses a serious threat of violence. This duty to protect overrides confidentiality in certain scenarios. It can save lives.
Privacy for clients is still very important. Mental health experts must weigh the need to protect with the need for privacy. They must act only when there is clear, immediate danger. This balance is critical to maintain trust and care in therapy.
When A Client Is A Minor
Mental health professionals often respect the confidentiality of their clients. Client conversations are private. Yet, specific scenarios require breaking this privacy rule. This is crucial when treating minors.
Parents generally have the right to know about their child’s mental health. Access can include session details and records. But there are exceptions.
Instances where parents may not access a child’s mental health information:
- If a court decides it is not in the child’s best interest.
- When the child is legally permitted to consent to their own treatment.
- If granting access would endanger the child.
State laws govern these exceptions. They protect the child’s well-being. Understanding these rules is important for both professionals and parents.

Credit: www.theraplatform.com
Privacy Breaches In Collaboration With Law Enforcement
Mental health professionals value client confidentiality greatly. Yet, certain conditions require these professionals to break this secrecy. One such situation is when they work with law enforcement. This typically happens in criminal cases or when handling forensic assessments.
Professionals might face the challenging task of balancing patient confidentiality with legal demands. Client information may only be shared if it pertains to a crime investigation or if it’s essential to public safety. For instance, if a client poses an immediate threat to themselves or others, the therapist may need to notify authorities. This action ensures safety for all.
Thus, communication with police usually happens under strict legal frameworks. Therapists must consult laws and regulations before sharing any details. They aim to protect their clients while also fulfilling their duty to society.
Public Health Emergencies And Privacy
Mental health professionals play a vital role during public health emergencies. These crises often raise tough questions about privacy rights. A significant challenge is balancing patient confidentiality with public safety. Privacy may be affected when a mental health issue poses a direct threat to others.
Epidemics or disease outbreaks can necessitate breaches in confidentiality. Disclosure may occur only for crucial reasons. One reason is to prevent a serious and imminent threat to public health. Mental health professionals must make difficult decisions swiftly. They protect individual privacy yet prioritize overarching public safety needs.
Ethical Dilemmas And Clinician Discretion
Mental health professionals face complex decisions regarding client confidentiality. Ethical guidelines provide a structure. Yet, gray areas often emerge. Situations arise where the law mandates disclosure. Instances include threats of harm to oneself or others. Child abuse or neglect cases also demand action.
Professionals may disclose information for legal proceedings. The clinician’s judgment plays a crucial role. They must weigh the potential harm of silence. The privacy of the client is always key. But safety and legal obligations can take precedence.
| Scenario | Action Required | Rationale |
| Threats to self | Report to authorities | Prevent harm |
| Threats to others | Warn potential victim | Prevent violence |
| Child abuse | Notify child protection services | Legally required |
Best practices suggest a risk-benefit analysis. Documentation and consultation with peers are critical steps. Confidentiality breaks should be a last resort. Client safety and welfare always guide these tough decisions.
Training And Policies To Ensure Compliance
Mental health professionals are bound by strict confidentiality policies. They undergo routine training on current legal standards. This ensures they understand when they can share information. Safeguards are critical to protect patient privacy.
Institutional safeguards involve several levels of protection. These include data encryption, secure communication channels, and access controls. Records are kept safe to prevent unauthorized access. Staff learns about privacy breaches and their impacts. They also learn how to avoid them. Trust is crucial in mental health care.
Credit: depts.washington.edu
Frequently Asked Questions Of Under What Circumstances Can Mental Health Professionals Break Confidentiality?professional?
Can Therapists Breach Patient Confidentiality Under Certain Circumstances?
Yes, therapists can breach confidentiality in certain situations. These include risks of harm to self or others, abuse reports, and legal requirements.
What Are The Exceptions To Confidentiality In Mental Health?
Confidentiality in mental health has exceptions such as suspected child abuse, threats of harm to self or others, and court orders. Certain infectious diseases may also mandate reporting.
What Are The 3 Reasons To Break Confidentiality?
Three reasons to break confidentiality include legal requirements, immediate harm risk, and client consent.
Under What Circumstances Can Mental Health Professionals Disclose Information Learned In The Course Of A Professional Relationship?
Mental health professionals may disclose information in situations involving threats of harm to self or others, abuse or neglect of children, dependent adults, or elders, and when legally required, such as court orders.
Conclusion
Ensuring patient privacy is critical in mental health care. Yet, there are exceptional situations where therapists may ethically divulge confidential information. These include imminent harm, legal requirements, or client consent. As clients, understanding these boundaries is paramount for trust in therapeutic relationships.
It’s vital to discuss confidentiality policies with your mental health professional to fully grasp their scope and limitations.